Abstract
Objective:
Ibrutinib is currently the most widely used BTK inhibitor that approved for the treatment of both initially diagnosed and relapsed and refractory chronic lymphocytic leukemia (CLL) patients. Although ibrutinib shows high response rates in clinical practice, it has certain limitations. There are still a certain number of patients who have to discontinue treatment due to drug-resistance or side effects. The ibrutinib resistance of CLL patients has caused widespread concerns, necessitating the development of novel treatment strategies.
Methods:
Here, we examined the heterogeneity of peripheral blood mononuclear cells (PBMCs) from patients with ibrutinib-sensitive (IBS) and -resistant (IBR) CLL by analyzing bulk and single-cell level gene expression profiles, clinical features, biological properties, and phenotypes. Seven distinct ibrutinib-resistant subpopulations were identified and two candidate genes LGALS1 (galectin 1, Gal-1) and LAG3 (lymphocyte-activating gene 3, CD223) were screened that contribute toward ibrutinib-resistance and poor survival in CLL patients. These results were validated in primary cells from CLL patients and also in ibrutinib-resistant CLL cell line (MEC1-IR) which was generated by culturing the parental cell line in vitro with progressively increasing concentrations of ibrutinib. Marker-gene expression was detected using qRT-PCR, western blotting, and ELISA, while functional analyses including CCK8, flow cytometry and trypan blue staining were conducted with or without OTX008, a selective Gal-1 inhibitor.
Results:
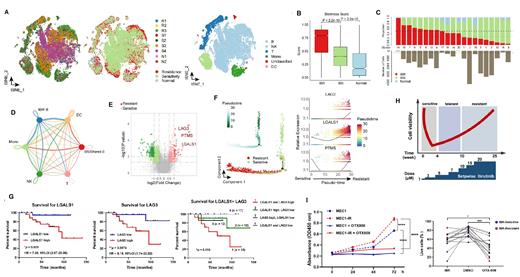
ScRNA-seq revealed that cells from IBR and IBS samples were distributed in different clusters and suggested that IBR cells display a unique transcriptional pattern (Fig A). IBR-B cells have higher stemness scores and are enriched in some energy metabolism
Pathways (Fig B). According to the proportion of B cells from IBR samples, we classified each B-cell cluster into three main subgroups, i.e., IBR, IBS, and shared cluster (Fig C). IBR-B cells displayed more interactions with monocytes, NK, T, and dendritic cells than IBS B cells, suggesting that IBR B cells may actively build connections with other immune cells to reshape the protective niche (Fig D). A close correlation between LGALS1 and LAG3 expression was observed and both of them were found to be highly expressed in IBR CLL patients (Fig E), their expression level gradually increased along the trajectory of B cells from IBS to IBR (Fig F). Diagnosis and prognosis stratification of CLL with receiver operating characteristic (ROC) curves revealed that patients with higher expression of both LGALS1 and LAG3 showed the poorest overall survival, indicating that LGALS1 and LAG3 are associated with ibrutinib-resistance and poor prognosis in CLL (Fig G). Concordantly, acquired resistance following chronic exposure to ibrutinib leads to upregulation of LGALS1 and LAG3 (Fig H). LGALS1 inhibitor OTX008 effectively inhibits the growth of ibrutinib-resistant CLL cells, particularly for IBR patients (Fig I).
Conclusion:
In conclusion, our findings demonstrate that ibrutinib-resistant CLL cells exhibit a unique transcriptional pattern. The combination of LGALS1 and LAG3 expression could serve as an indicator of the sensitivity of ibrutinib and prognosis of CLL patients. LGALS1 inhibitor OTX008 helps to overcome ibrutinib-resistance of CLL cells. Our findings may expand the current knowledge regarding ibrutinib-resistant CLL patients, identify improved biomarkers for patient selection, and offer a promising combinatorial therapeutic strategy for IBR CLL patients.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal